Antibiotic Use In Pets- A True Lifesaver!9 min read
ANTIBIOTIC USE IN PETS SAVES LIVES
If you were to name one thing that has saved the lives of multitudes of humanity and their companion animals it would have to be antibiotics. Antibiotics have not even been around for a century. The first antibiotic, penicillin, was discovered in the mid 1920’s by Fleming. Prior to that people and animals died of simple bacterial infections that we don’t even think much about today. The casualties of wars over the years were greater because antibiotics had not been discovered. These people died of the complications of bacterial infections such as gangrene and sepsis. The black plaque in Europe around 1300 AD wiped out most of the population of the continent. The plaque is caused by a bacteria (Yersinia pestis). Imagine if antibiotics had been available then! Antibiotic use has allowed pets and their human masters to survive many life threatening bacterial diseases.
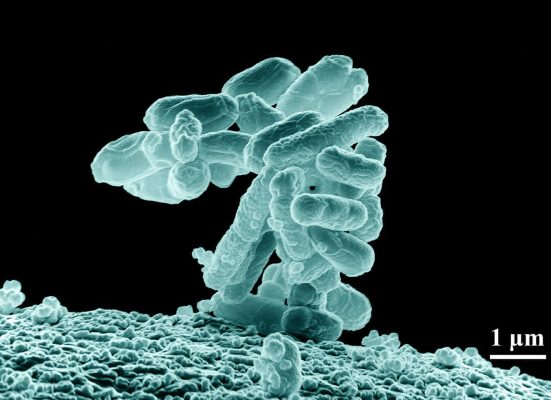
Antibiotics are also known as antibacterials. The terms are synonymous with one another. Antibiotics only work against bacteria. Antibiotics have ZERO effect on viruses!! They work in the most part by destroying the cell wall of the bacteria. This causes immediate cell death. This is what E. coliThe complete name for E. coli is Escherichia coli. It is much easier to remember E. coli. In undergrad you would be docked for misspelling bacterial names on exams. E. coli is a Gram negative rod bacteria that causes death from sepsis and renal failure. looks like under an electron microscope:
All bacteria are invisible to the naked eye. As I have said a multitude of times in my career is that the things you can’t see can and will kill you. The appropriate antibiotic use in pets is lifesaving. I knew in high school I was going to end up in a medically related field. In high school I took every science course except advanced physics. In biology II we plated out bacteria on a petri dish. We let the bacteria grow. We were then told to bring a sample of dirt from home. We sprinkled dirt on the bacteria. Less then a week later there were clumps of fungi growing with circular, clear areas that were devoid of bacterial growth! These fungi grow and secrete substances that destroyed bacteria. I witnessed the manufacture of antibiotics in front of my own eyes. I was hooked. It is no wonder that my undergraduate degree from The Ohio State University was in Microbiology.
THE DEVELOPMENT OF THE ANTIBIOTIC FAMILY
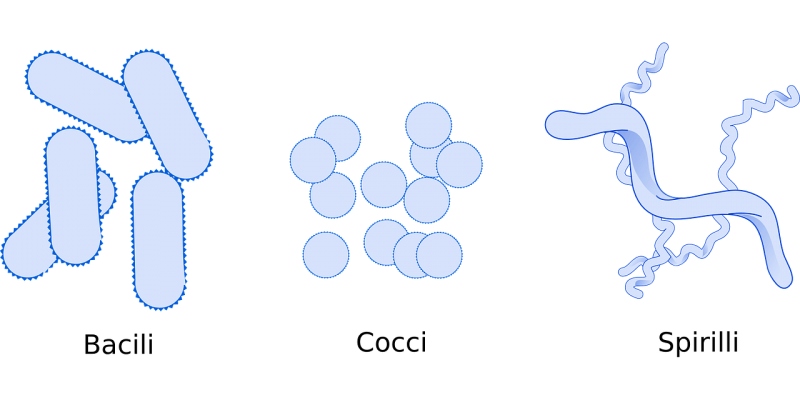
There was one major problem with Penicillin. It was a fantastic new drug but it was only effective against certain types of bacteria. It could do nothing against many other bacterial agents that cause disease. There are three types of bacteria as shown above. E. coli is an example of a bacili (rod) bacteria. Streptococcal pneumonia is an example of a cocci bacteria. Syphilis (Treponema pallidum) is an example of a spiral bacterial organism. Over decades of medical research other drugs became available that are known as “broad spectrum” antibiotics. These are antibiotics that take care of the majority of cocci and rod bacteria. Examples of this are ampicillin and amoxicillin. Broad spectrum antibiotic use in pets has been shown to take care of the majority of bacterial infections.
Today there are many high tech broad spectrum antibiotics that medical practitioners use on a daily basis. Examples of these are: advanced penicillins such as Clavamox® (Augmentin® in human medicine), cephalosporins such as Keflex®, quinolones such as Baytril® or Zeniquin® and Macrolides such as Zithromax®. Antibiotic use in pets means that you don’t necessarily have to use the latest and greatest to treat a basic infection. This will be delved into later on. The take away point is that antibiotic use in pets keep the ravages of bacterial disease under control.
HOW ARE ANTIBIOTICS USED?
Antibiotic use in pets is effective when the clinician is suspecting a bacterial cause of disease. Examples of this are: ear infections, skin infections, urinary tract infections and intestinal infections. The uses of antibiotics in daily practice are limitless. When there are severe bacterial infections present veterinarians will often use a combination of antibiotics to get an infection under control. This is often the case when there is little or no time to do a bacterial culture. An example of this is pyometra; a severe uterine infection in dogs and cats. Veterinarians may grab a culture when they are in surgery but will initially use combinations of antibiotics to help get the animal back on its feet (paws).
Antibiotic use in pets can be accomplished in several ways:
- Orally- This is the simplest route for animals unless you own a cat. Cats hate to be pilled and will sometimes tolerate liquids. Oral use of antibiotics is contraindicated in animals that are vomiting. Certain antibiotics such as Clavamox® (Augmentin®) can irritate the stomach lining in animals with a pre-existing intestinal infection.
- Subcutaneal or Intramuscular– Dogs and cats have loose skin so drugs can be administered under the skin (subcutaneal) or intramuscular. This route of administration has been a godsend for cat owners. Many cats will fight over ANY oral preparation. For those persnickety cats all veterinarians will give a subcutaneous injection of Convenia®; a 2 week lasting cephalosporin antibiotic. The subcutaneous or intramuscular route is quicker acting than an oral product.
- Intravenous- Many antibiotics come in a liquid form that may be injected directly into the bloodstream. These are the fasting acting antibiotics.
- Ointments- These topical preparations are often only used in ear infections. Most ointments applied to the skin of animals will be licked off. Topicals are great and if needed an Elizabethan collar is applied around the pet’s head.
- Nebulizer- Many bronchitis and or pneumonia patients benefit from breathing in steam that is fortified with lots of goodies that make it easier to breathe. Liquid antibiotics are put in the nebulizer mix and easily reach the respiratory tree by direct inhalation of the drug.
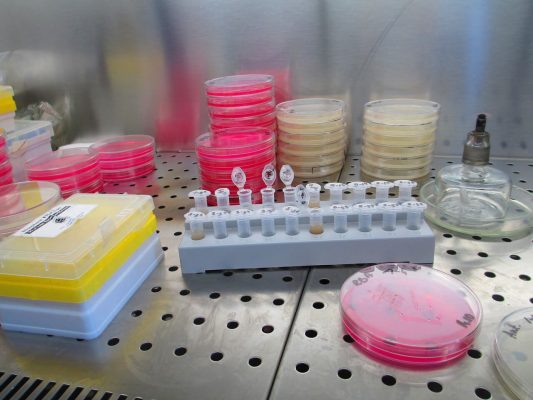
Many veterinarians will do a culture and sensitivity test to find the right antibiotic for your dog or cat. We all use drugs that knock out the most common bugs in dogs or cats. Sometimes that does not work. Rather than guessing which antibiotic to use we take cultures of whatever is in question and send it to a lab. The lab grows the bacteria and tells the clinician which antibiotic(s) will cure the infection. A typical lab that does this work looks like this:
Antibiotics do not work against any virus. Paradoxically, antibiotics are always used in these cases in cats. They have nothing to do with the virus but what viruses do to the body. All viruses suppress the immune system. This same logic is often used when people say they “got the flu again”. This is impossible. What they got was another viral or bacterial infection SECONDARY to the immune suppression of the flu virus. Respiratory infections in cats are all caused by viruses (herpes virus, calicivirus, rhinotracheitis). Viruses will suppress the cellular immune system allowing secondary bacterial infections to take hold. This is why cats respond so well to amoxicillin or cephalosporin administration.
THE THREAT OF ANTIBIOTIC RESISTANCE
This is the 3000 pound elephant in the room. Bacteria have been resistant to certain antibiotics for a long time. In the past this meant switching to another class of antibiotics that would do the job. What happens when we run out of other classes of drugs to use? We are very close to this in veterinary and human medicine. Antibiotic use in pets or the effectivity of these drugs in pets would come to a screeching halt. Take heed to the recent press release of a super bug (E. Coli) that was found in a Pennsylvania woman this past week. It is resistant to just about everything. That is dangerous.
All living creatures (including bacteria) have DNA. Some viruses have RNA. Regardless, it carries all the genetic material of the individual. DNA is made from nuclei acids that are paired in a certain way so that a trait (gene) or a mutation is expressed. That double helix DNA looks something like this:
These mutations or changes in bacteria are accomplished or produced in several ways:
- Over usage of new antibiotics- Many times a simple antibiotic such as a cephalosporin will do the job instead of a super antibiotic. The key is to use these new drugs ONLY when you have to!
- Under dosage of new antibiotics- Not using the appropriate dose of any antibiotic will lead to bacterial resistance over time.
- Antibiotics not used long enough- If the infection is not cleared by XYZ days a sub-clinical case of the bacterial infection will set up shop. These can mutate to produce resistant bacteria.
I personally preached this to the choir decades ago when Baytril® hit the veterinary market. It was a spectacular quinolone antibiotic. I asked the drug representative what was going to happen when everything was resistant to that drug? No answer. Today many bacteria are resistant to Baytril®. I have done countless amounts of cultures in my career and my ears perked up when I started seeing resistance to the drug. Yes, there are other antibiotics that will work but resistance is usually caused by one of the above mechanisms.
Antibiotic use in pets is necessary and saves lives. The million dollar question is this: What do we do when nothing works?